Abstract
Background: Sexually transmitted infections (STIs) constitute a major public health problem worldwide. They are important because of their magnitude, potential complications, and interactions with HIV/AIDS. Due to this fact, the National HIV/AIDS Policy of Ethiopia identified STI prevention and control as one of the strategies to prevent and control HIV/AIDS. In order to fill the critical information gap on STI, Ethiopian Public Health Institute (EPHI) has established a national STI surveillance system in selected sentinel health facilities.
Method: From July 2014 to June 2015, a cross sectional study was carried out in 20 sentinel health facilities to determine the proportion of respondent with Urethral discharge, Vaginal discharge, Lower abdominal pain, Inguinal Bubo, Scrotal swelling, Genital ulcer disease and their HIV status.
Result: The majority (67%) of the participants was in the age group 20-34 yrs and 68% of them were females. From 1421 participants, 1333 were diagnosed with one symptom and 88 with two symptoms; vaginal discharge constitutes the highest proportion (52.2%) followed by urethral discharge (25.3%), then lower abdominal pain (13.3%), non-vesicular GUD (4.6%) and vesicular GUD (2.7%).
The participant’s sexual history for the past three months was assessed and 17.4% of them had sexual encounter with a non-regular partner and of them 55.8% have not used condom with non-regular partner during the last contact. In addition, HIV status was reported by 1118 (78.7%) participants and 181 (16.2%) of them were found to be HIV positive (8.4% among males and 19.7% among females). Out of 107, HIV positive study participants, who reported their previous HIV status, 88 (82.2%), used to know their HIV status and 19 (17.8%), were newly tested positives.
Conclusion: Our findings indicate that a considerable proportion of patients had sexual encounter with a non-regular partner in the last three months period and of them more than half have not used condom during the last sexual contact. Moreover, a larger proportion of HIV positive STI patients used to know their status before the study. Therefore, expansion of STI preventive services including health education on the transmission and possible complications of untreated STI is crucial.
Keywords
Sexually transmitted infection; Syndromic management; HIV; Risk factors; Ethiopia
Abbreviations
ART: Antiretroviral therapy; CDC: Communicable disease control; EPHI: Ethiopian public health institute; GUD: Genital ulcer disease; GUDV: Genital ulcer disease vesicular; HMIS: Health management information system; HIV: Human immune deficiency virus; ING: Inguinal Bubu; LAP: Lower abdominal pain; OPD: Out patient department; RHB: Regional health bureau; STI: Sexually transmitted infection; SS: Scrotal swelling; SNNPR: Southern nation, nationality and people region; UD: Urethral discharge; VD: Vaginal discharge; VCT: Voluntary counseling and testing.
Background
Sexually transmitted infections (STIs) constitute a major public health problem worldwide especially in developing countries. An estimated 357 million new cases of curable sexually transmitted infections, mainly due to Treponema palladium (syphilis), Neisseria gonorrhea, Chlamydia trachomatis, and Trichomonas vaginalis, occur every year throughout the world in men and women aged 15–49 years [1]. Moreover, the impact of these diseases is magnified by their potential to facilitate the spread of human immunodeficiency virus (HIV) [1].
Cognizant of these facts, the National HIV/AIDS Policy of Ethiopia identifies STI prevention and control as one of the strategies to prevent and control HIV/AIDS [2]. However, nationally there is still considerable underreporting of STI cases. Underreporting has been due to excessively long list of reportable diseases; concerns about confidentiality; provision of treatment by the informal sector; the asymptomatic nature of some STIs and the fact that there is no strong Syndromic Case Management Program in all the regions of the country, even though Ethiopia has adopted the syndromic approach to manage STI cases [2].
In Ethiopia, any patient who presents with STI case in health facilities is treated by syndromic approach. The main reason for the development of STI syndromic approach is not only lack of skilled health professionals’ rather inadequate access to laboratory for etiological diagnosis; it is only syphilis testing which is being conducted by laboratory investigation. The syndromic approach has its guideline and every health professional takes training on how to manage STI cases [3].
Nevertheless, much remains to be done in strengthening the STI prevention and control program in the country. One of the most outstanding problems is lack of information on the status and trends of STIs in the country.
Therefore, the main objective of this study is to estimate the magnitude of the six priority reportable STI syndromes (urethral discharge, genital ulcer, vaginal discharge, lower abdominal pain in women, inguinal bubo and, scrotal swelling) and generate additional information on selected demographic and behavioural variables and determine the HIV status of study participants.
Methods
Study design
From July 2014 to June 2015, a cross sectional study was carried out in 20 sentinel health facilities to determine the proportion of respondents with Urethral discharge, Vaginal discharge, Lower abdominal pain, Inguinal Bubo, Scrotal swelling, Genital ulcer disease and their HIV status.
Selection of study participants
The study sites were selected from health centres and hospitals across the country. Any client, who is newly diagnosed and/or treated as a case of STI in the general outpatient department (OPD), in the STI unit, Antiretroviral therapy (ART) room, and in the youth friendly service unit was included in the sampling.
Data collection tools
The data-collecting format contains 15 variables including sociodemographic, risk factors and HIV status. The questionnaire was adopted from WHO recommendation for STI studies [4]. The health professionals (medical doctor/Nurse/Health officer) collected the Data and filled the required information on the data collecting form for every consecutive STI patient with new symptom. Data was entered using CSPRO software and the analysis and tabulation of data was made using SPSS version 20. Trainings were given on data collection, handling, and reporting for regional coordinators and site level staffs using standardized-training manuals. Every month the collected data was submitted to the investigator through the assigned coordinators.
Study variables
The diagnosis of STIs relies on proper history taking and physical examination. For each syndrome, a clinical flow chart is developed for STI case management. A flow chart (also known as an algorithm) is a decision and action tree, which is like a map that guides the health worker to go through a series of decisions and actions [3].
Urethral discharge in men: is the presence of abnormal secretions from the distal part of the urethra and it is the characteristic manifestation of urethritis; can also have increased frequency and urgency of urination and itching sensation of urethra.
Vaginal discharge in women: when a women notices abnormal vaginal discharge (a change in color, odor, and amount accompanied by pruritus).
Genital ulcer in men and women: is an open sore or a break in the continuity of the skin or mucous membrane of the genitalia because of sexually acquired infections.
Lower abdominal pain in women: refers to a clinical syndrome resulting from ascending infection from the cervix and/or vagina. The syndromes are presence of vaginal discharge, Inter-menstrual or post coital bleeding, and systemic symptoms like fever, nausea, and vomiting.
Scrotal swelling in men: the signs and symptoms of scrotal swelling are pain and swelling of the scrotum, tender and hot scrotum on palpation, edema, and erythema of the scrotum and history of concomitant urethral discharge.
Inguinal Bubo in men and women: is defined as swelling of inguinal lymph nodes because of STIs. The signs and symptoms are a classical “groove sign” in the inguinal area, fluctuant abscess formation, fever, headache and pain.
Results
Socio-demographic characteristics of the respondents
A total of 1421 individuals from 20 health facilities have participated in the study. Majorities (62.8%) of the study participants were in the age group of 20-34 yrs with a mean age of 26 yrs and 68.2% were females. Majority (66.6%) of the patients had educational status of 8th grade or less, only a small proportion (7.2%) attended above 12th grade. About 51.3% of the respondents were married and 15.4% of participants were daily laborers (Table 1).
| Characteristics |
Frequency |
Percent (%) |
| Age |
| <24 |
512 |
13.9 |
| 25-34 |
572 |
53.7 |
| 35-44 |
193 |
22.7 |
| 45+ |
76 |
6.3 |
| Missing |
68 |
3.3 |
| Total |
1,421 |
100 |
| Sex |
| Male |
441 |
31 |
| Female |
968 |
68.1 |
| Missing |
12 |
0.8 |
| Total |
1,421 |
100 |
| Educational status |
| No Formal |
387 |
27.2 |
| Grade 1-4 |
262 |
18.4 |
| Grade 5-8 |
298 |
21.0 |
| Grade 9-12 |
274 |
19.3 |
| Higher |
103 |
7.2 |
| missing |
97 |
6.8 |
| Total |
1,421 |
100 |
| Marital status |
| Never Married |
447 |
31.5 |
| Currently Married |
729 |
51.3 |
| Widowed |
49 |
3.4 |
| Divorced/ Separated |
111 |
7.8 |
| Unknown |
9 |
0.6 |
| missing |
76 |
5.9 |
| Total |
1,421 |
100 |
| Occupation |
| Sex Worker |
38 |
3.9 |
| Military |
27 |
2.8 |
| Vehicle Driver |
36 |
3.7 |
| Daily Laborer |
148 |
15.4 |
| Mobile Merchant |
41 |
4.3 |
| Farmer |
136 |
14.1 |
| Gov't Employee |
106 |
11 |
| Self Employed |
97 |
10.1 |
| Other Occupations |
335 |
34.8 |
| Gross Total |
964 |
100 |
Table 1: Socio-demographic characteristics of the study participants, July 2014-June 2015
Pattern of reported STI syndromes
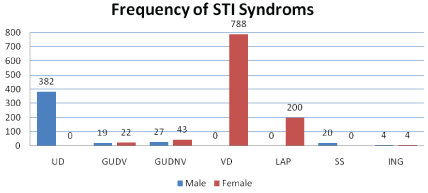
A total of 1509 (452 from male and 1057 from female) STI syndromes were identified; majority (88%) of them only had one syndrome while 88 (12%) were diagnosed with two syndromes. Regarding the proportion of all syndromes, vaginal discharge consists the highest proportion (52.2%) followed by urethral discharge (25.3%) (Figure 1). Analysis of the STI cases with age-disaggregation showed that 42.3% fall under 24-34 yrs age group (Table 2).
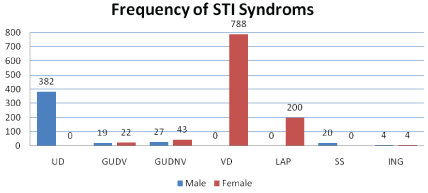
Figure 1: Frequency of STI syndromes categorized by Sex in Ethiopia, July 2014-June 2015
UD: Urethral discharge ; VD: Vaginal discharge; ING: Inguinal Bubu; LAP: Lower abdominal pain; GUD: Genital ulcer disease; SS: Scrotal swelling; GUDV: Genital ulcer disease vesicular
| STI Syndrome (Yes) |
Total Men+Female |
Male |
Female |
| <24 N |
24-34 N |
>34 N |
Total Men |
<24 N |
24-34 N |
>34 N |
Total Female |
| UD |
365 |
137 |
163 |
65 |
365 |
|
|
|
|
| GUDV |
38 |
7 |
6 |
3 |
16 |
6 |
12 |
4 |
22 |
| GUDNV |
68 |
6 |
14 |
5 |
25 |
18 |
17 |
8 |
43 |
| VD |
746 |
|
|
|
|
303 |
295 |
148 |
746 |
| LAP |
189 |
|
|
|
|
51 |
90 |
48 |
189 |
| SS |
20 |
6 |
10 |
4 |
20 |
|
|
|
|
| ING |
8 |
1 |
2 |
1 |
4 |
1 |
3 |
|
4 |
| HIV-Positive |
170 |
4 |
12 |
13 |
29 |
15 |
79 |
47 |
141 |
Table 2: Frequency of STI syndromes and HIV status categorized by sex and Age Group, July 2014 - June 2015
The total number of STI syndrome might decrease in number due to missing age data.
UD: Urethral discharge; VD: Vaginal discharge; ING: Inguinal Bubu; LAP: Lower abdominal pain; GUD: Genital ulcer disease; GUDV: Genital ulcer disease
vesicular; SS: Scrotal swelling
Risk behavioral factors of STI patients
Majority of the respondents (62.3%) claim to have only one sexual partner while 14.3% reported two or more sexual partners and 17.4% of the participants had sexual encounter with non-regular partner in the last three months period. Majority (55.8%), who had sexual contact with a non-regular partner, have not used condom during the last sexual contact (Table 3).
| Risk behaviors |
Total N (%) |
Male N (%) |
Female N (%) |
| Number of sexual partners in the past three month |
| 0 |
299 (23.4) |
82 (27.4) |
217 (72.6) |
| 1 |
795 (62.3) |
222 (27.9) |
573 (72.1) |
| >1 |
182 (14.3) |
97 (53.3) |
85 (46.7) |
| Total |
1.276 |
401 |
875 |
| Sex with non-regular partners in the past three month |
| Yes |
239 (17.4) |
143 (59.8) |
96 (40.2) |
| No |
1,131 (82.6) |
282 (24.9) |
849 (75.1) |
| Total |
1,370 |
425 |
945 |
| Condom use during last sex with non-regular partner |
| Not Used Condom |
130 (55.8) |
78 (60) |
52 (40) |
| Used Condom |
103 (44.2) |
60 (58.3) |
43 (41.7) |
| Total |
233 |
138 |
95 |
| Pregnancy |
| Total |
946 |
- |
64(6.8) |
Table 3: Risk Behavioural factors of STI patients, July 2014–June 2015
STI patients with pregnancy status
Out of 946 female participants whose pregnancy status was checked, 64 (6.8%) were at some stage of pregnancy (Table 3). The pregnancy status was reported by the clients and supported with physical examination and laboratory diagnosis.
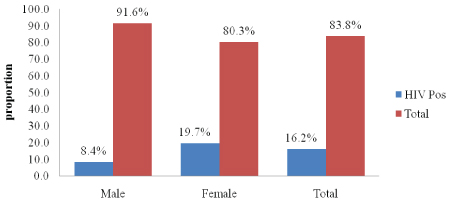
HIV prevalence among STI patients
The HIV status of 1118 study participants was documented and of them 181 (16.2%) were found to be HIV positive (8.4% among males and 19.7% among females). Among 107 HIV positive study participants, whose previous HIV status was documented, 88 (82.2%) knew that they were HIV positive and 19 (17.8%) were newly identified positives during the study (Figure 2). Furthermore, higher HIV prevalence was observed among patients with vesicular GUD (32%) and ING (28%) Syndrome. HIV prevalence also showed the same demographic pattern with other STIs, majority of HIV positive study participants (53%) lay between the age group of 24-34 (Tables 2 and 4).
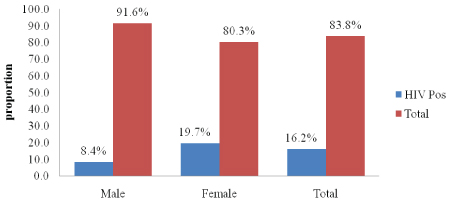
Figure 2: Proportion of HIV positive study participants categorized by sex in Ethiopia, July 2014 – June 2015
|
STI Syndrome |
Male |
Female |
| HIV-positive N (%) |
HIV-Negative N (%) |
HIV-positive N (%) |
HIV-Negative N (%) |
| UD |
23 (7.8) |
271 (92.2) |
|
|
| GUDV |
3 (17.6) |
14 (82.4) |
9 (45) |
11 (55) |
| GUDNV |
1 (4) |
23 (96) |
9 (27.3) |
24 (72.7) |
| VD |
|
|
121 (18.9) |
518 (81.1) |
| LAP |
|
|
21 (13.7) |
132 (86.3) |
| SS |
2 (11.1) |
16 (88.9) |
|
|
| ING |
0 |
3 (100) |
2 (50) |
2 (50) |
Table 4: STI syndromes disaggregated by HIV status, July 2014-June 2015
UD: Urethral discharge; VD: Vaginal discharge; ING: Inguinal Bubu; LAP:
Lower abdominal pain; GUD: Genital ulcer disease; GUDV: Genital ulcer
disease vesicular; SS: Scrotal swelling
Discussion
The study has shown that 67% of the participants were in the age group 20-34 yrs and 68% of them were females. Regarding the syndrome vaginal discharge constitutes the highest proportion (52.2%) followed by urethral discharge (25.3%). In addition, 181 (16.2%) of the participants were HIV positive (8.4% among males and 19.7% among females).
Reported STIs represents only the “tip of the iceberg”, because most infections typically more than half of any specific diagnosis regardless of bacterial or viral etiology, are entirely asymptomatic or unrecognized, this is especially true for women [5,6]. This obviates that the actual situation in the study area could even be worse as only symptomatic cases came to the clinic. There could also be unreported symptomatic cases due to stigma and discrimination, fear of potential conflict with sexual partner especially in the married group, self-prescription of medicines from pharmacies, preference to traditional healers, and because of the general poor health seeking behaviour of the community [7].
In 2015, WHO reported a global estimate of 357 million new cases especially by four curable STIs (syphilis, gonorrhoea, Chlamydia and trichomoniasis) in adults aged 15-49 years [8]. In addition, younger age group (15-24 yrs), even though they represent only 25% of sexually active population, they consists almost 50% of the new acquired STIs [9]. Our study also showed that young people in the age group of 20-34 yrs are the most affected with a larger proportion of females. The result is in agreement with the report by Klouman et al. [10] in Tanzania and Kassa et al. [11] in Southern nation, nationality and people region (SNNPR). Men and women have different susceptibility to STI due to biological vulnerability; one of the reasons for the difference is the contact period with pathogens after sexual exposure, it is more extended among women than men are. That is, if the male partner has an STI, the infected semen remains in the vagina following intercourse; in contrast, if the female partner is infected, the male’s exposure to the pathogens is limited to the duration of coitus [12]. The cervix may also be more susceptible to infection than the male’s urethra. Furthermore, STIs are asymptomatic in women than in men [12].
The most frequent STI syndromes reported for women were vaginal discharge and urethral discharge for men; this is consistent with the study done by Kassa et al. [11] in SNNPR and Beyene et al. [7] in Gondor town, they reported 55.7% and 38.38% vaginal discharge and 25.8% and 13.58% urethral discharge, respectively.
The Proportion of study participants with vesicular and non-vesicular ulcer disease were 7.4%, which is almost similar with the study done in SNNPR (6%) [11]. Genital ulcer diseases serve as a proxy for important curable bacterial STIs, such as syphilis and chancroid, as well as for incurable viral STIs such as herpes simplex virus [13-15]. Where most genital ulcer cases are due to curable bacterial STI, strengthening management of STIs should lead to a decline in rates of genital ulcer cases. The proportion of study participants with UD was 25%. It indicates the need for carefully assessing STI control efforts in the country.Urethral discharge among males is another key indicator, which shows the strength of STI control programs, in countries without strong STI laboratory capacity [13].
Different behavioral risk factors have been frequently associated with sexually transmitted infections [14]. This study also showed that 17.4% of patients had sexual encounter with a non-regular partner in the last three months period and around 55.8% of them have not used condom during the last sexual contact with anon-regular partners. In addition, 14.3% of the patients had two or more sexual partners in the last three months, which calls for a need to strengthen our effort in health education activities. Health care providers and community health workers should focus on behavior change intervention such as safer sexual practices and condom use [16].
Out of female study participants 6.8% were at some stages of pregnancy, effort should be made to prevent and treat STIs during pregnancy, as untreated sexually transmitted infections are associated with congenital and prenatal infections in neonates, particularly in areas where rates of infection remain high. WHO reported that in pregnant women with untreated early syphilis, 25% of pregnancies result in stillbirth, 14% in neonatal death, and an overall prenatal mortality of about 40%. Up to 35% of pregnancies among women with untreated gonococcal infection result in spontaneous abortions and premature deliveries, and up to 10% in prenatal deaths [15]. This emphasizes the need for effective interventions involving community health workers on house-to-house health education program and strengthening STI case identification at antenatal care units.
HIV prevalence among study participants was 16.2% (8.4% among males and 19.7% among females). Most HIV positive participants knew their status at study entry. Hence, Health care providers need to work more on awareness creation towards safer sexual practice including condom use for HIV positive individuals to decrease exposure to other STIs.
The potential for HIV transmission is increased by the presence of STIs, and ulcerative STIs by breaking off the body’s most important defense (skin/mucosal membranes) [17]. In this study, patients with Genital ulcer syndrome had the highest HIV prevalence (32.4%). A cohort study done in Zimbabwe and Nigeria, showed the role of genital ulcerative conditions in male to female transmission of HIV; Men who reported a history of genital ulcer disease were more likely to have HIV (RR 1.94 (1.62- 15.13)) [18,19].
Conclusion
Our findings indicate that a considerable proportion of patients had sexual encounter with non-regular partner in the last three months period and more than half of them have not used condom during the last sexual contact. Moreover, a larger proportion of HIV positive STI patients used to know their status before the study. Therefore, expansion of STI preventive services including health education on the transmission and possible complication of untreated STI is crucial. Appropriate health care seeking behavior, information education and communication activities should also be strengthened.
Limitation
This study was conducted in twenty selected health facilities across the country, which does not assume neither regional nor national representativeness; therefore, care should be taken not to generalize these study findings to respective regional or national program performance.
Declarations
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Ethics Approval and Consent to Participate
Ethiopian public health institute and CDC ethical review board approved the survey. Before filling the data collection form, the professionals obtained verbal consent that appears at the back of the reporting form. Any client information was confidential throughout the processes. Reporting formats and patient registers were kept in locked rooms and the health professionals who were involved in the data collection and compilation were trained on confidential handling of data. The participants also consented to use the data for further analysis and reporting to the scientific community.
Consent for Publication
Not applicable.
Availability of Data and Materials
Data and materials will be shared based on EPHI data sharing policy.
Competing Interests
The authors declare that they have no competing interests.