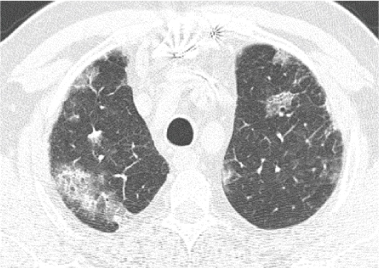
Figure 1: Axial section of CT scan showing foam of alveolar condensation and frosted glass.


M Kechida1* Ksiaa I2 K Ben Rhouma3 N Zaafrane2 S Khochtali2 M Khairallah2
1Internal Medicine and Endocrinology Department, Fattouma Bourguiba Hospital, University of Monastir, Tunisia*Corresponding author: M Kechida, Internal Medicine and Endocrinology Department, Fattouma Bourguiba Hospital, University of Monastir, Tunisia, E-mail: kechida_mel_lek@hotmail.com
Granulomatosis with Polyangiitis (GPA) is a systemic vasculitis characterized by upper and lower respiratory tract involvement with renal manifestations. Bronchiolitis Obliterans Organizing Pneumonia (BOOP) can be a misleading pulmonary manifestation especially in the onset of the disease, in the absence of the other major findings of GPA which can develop later during the follow up. Malignancy occurrence seems to be increased in GPA patients due to treatment but other authors reported an increase of preceding cancers too. We reported a case of BOOP in the onset of GPA associated with orbital pseudo tumor and prostatic cancer.
Granulomatosis with polyangiitis; Prostatic neoplasm; Cryptogenic organizing pneumonia; Orbital pseudotumor
Granulomatosis with Polyangiitis is a rare multi system vasculitis of presumed auto immune origin with a predilection for the ear throat and nose, lungs and kidneys [1]. Clinical manifestations are variable and in some extent ambiguous making the diagnosis sometimes difficult. Pulmonary findings are usually nodules evolving to the excavation [1]. BOOP was rarely reported as a minor manifestation of GPA [2]. Having this affection in the onset of the disease can be a misleading manifestation in the absence of other clinical findings and antibodies to Neutrophil Cytoplasmic Antigen (ANCA) positivity.
Malignancy occurrence was reported in the course of GPA as a result of Cyclophosphamide treatment. Other authors suggest a trigger role of cancers for GPA. Here we report a rare case of GPA revealed by BOOP associated with orbital pseudo tumor and prostatic cancer to highlight the importance of knowing such clinical manifestations at the onset of the disease and to discuss such association.
A 73 year old man with a history of coronary artery bypass grafting, implanted with pace maker was admitted in the internal medicine department for inflammatory arthralgia, myalgia, anorexia and weight loss evolving since 2 months. He reported to be treated 2 months ago for Bronchiolitis Obliterans Organizing Pneumonia (BOOP) (Figure 1) with 0.5 mg/kg/day of steroids for 2 weeks, than tapered with good outcome. On examination, there was no arthritis, no muscular deficiency, no lymph nodes or splenomegaly. Pulmonary auscultation revealed few crackles on the bases. Chest x-ray showed interstitial appearance. Biologic finding showed inflammatory syndrome with elevated erythrocyte sedimentation rate at 110 mm and C reactive protein at 22 mg/l. There was no cytolysis or cholestasis, no renal insufficiency, no hematuria, no anemia and no hyper leukocytosis. Prostate specific antigen was elevated leading to performing a body Computed Tomography (CT) scan showing definitive fibrosis associated with BOOP (Figure 2) and heterogeneous aspect of the prostate with no other secondary lesions.
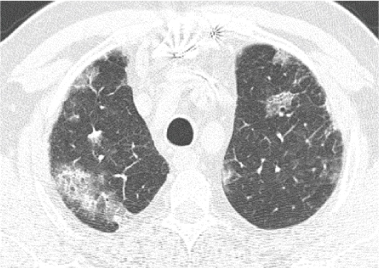
Figure 1: Axial section of CT scan showing foam of alveolar condensation and frosted glass.
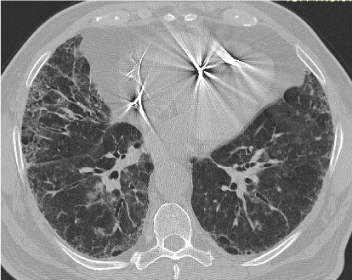
Figure 2: Cross section CT scan with sub-pleural dual-basal honeycomb lesions with septal and intra-lobular cross-linking, predominantly straight showing definitive fibrosis installed associated with BOOP.
Two days later, the patient complained of red and painful Right Eye (RE) associated to vertical diplopia (Figure 3). On ophthalmic examination, the patient presented right eye proptosis, upper lid swollen and erythema. Extraocular muscle examination revealed restriction of RE lateral, medial and downgazes with pain associated with ocular movement. Best Corrected Visual Acuity (BCVA) was 20/80 in his both eyes. Slit lamp examination showed conjunctival hyperemia, chemosis, exacerbed in the upper rectus and lateral rectus muscle insertion. The rest of the eye examination was unremarkable except of a bilateral dense cataract.

Figure 3: The patient presenting right eye proptosis, upper lid swollen and erythema.
A cerebral and facial CT scan showed the aspect of orbital right myositis with nodules of the nasal mucosa associated with osteolysis of the nasal septum (Figure 4a-4b).
Antinuclear anti cytoplasmic antibodies were positive type Proteinase 3 (PR3). The patient was diagnosed as having granulomatosis with poly angiitis and treated with 3 pulses of steroids associated to Cyclophosphamide with a good outcome of the ophthalmic swelling. We performed than a nasal and prostatic biopsy. The former showed no vasculitis nor granuloma and the latter showed prostatic adenocarcinoma.
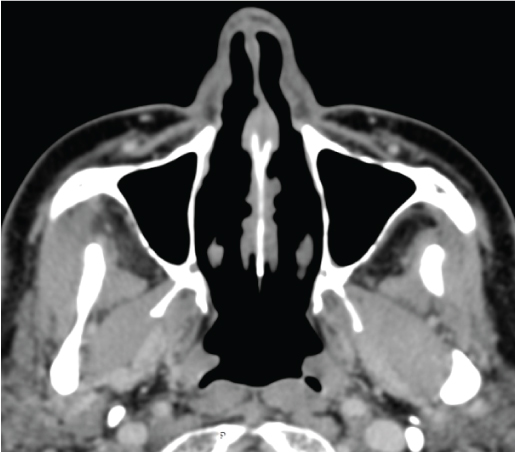
Figure 4a: Axial section of CT scan of the facial mass showing nodules of the nasal mucosa.
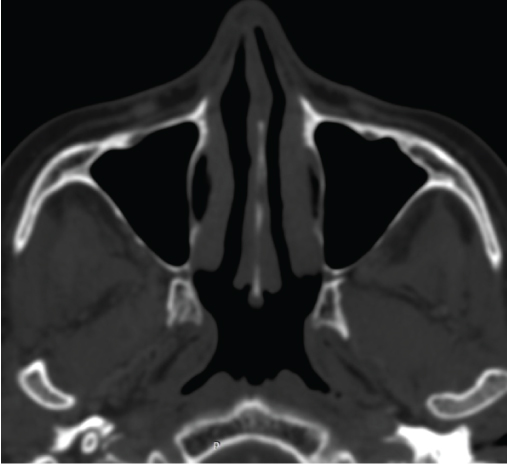
Figure 4b: Axial section of CT scan, bone window: osteolysis of the nasal septum.
We reported a case of granulomatosis with polyangiitis revealed by BOOP and orbital inflammatory pseudo tumor associated with prostatic adenocarcinoma. Granulomatosis with polyangiitis is a multisystem vasculitis which predominantly affects small caliber arterial vessels. It usually involves the upper and the lower respiratory tracts with kidneys. antibodies to neutrophil cytoplasmic antigen seem to play a role in the pathogenesis of the disease.
Pulmonary involvement of GPA can reach 50% to 75% of the cases [1]. It can be variable ranging from a simple cough to intra alveolar hemorrhage. The most specific lesions are multiple thick wall lung nodules sometimes excavated [1] revealing in histopathology findings necrotizing vasculitis with granuloma. BOOP is another pulmonary finding less frequently reported in patients with GPA. It is described to be one of the minor pathologic findings in GPA by Travis et al. [2] in addition to interstitial fibrosis, alveolar hamorrahage, tissue eosinophils and other variety of bronchiolar lesions. Travis and coworkers [2] reported BOOP in 31% of their patients with GPA. Whether the diagnosis of BOOP is radiological or histological, the diagnosis of GPA can be delayed in the absence of other criteria of the disease. In our case it is the onset of the ocular manifestation and the orbital CT scan findings which guided us to request ANCA.
Ophthalmic manifestations in GPA can occur in 28% to 87% of the patients [3]. Orbital involvement can occur in 15 to 20% of the cases. Clinically it can lead to proptosis, diplopia and in severe cases to optic nerve ischemia [3]. Orbital involvement can result from primary orbital inflammation or spread from adjacent paranasal sinuses or nasopharynx [3]. It is more frequently unilateral than bilateral but can be sight threatening if not treated early in case of optic nerve compression.
The diagnosis of GPA is still based on the American College of Rheumatology (ACR) criteria [4] (Table 1) which include only clinical, radiological or histological findings and do not take into account ANCA positivity with PR3 specificity which are reported to have a pooled sensitivity of 91% and a specificity of 99 % of active GPA [4]. In practice, only half cases of nasal sinus biopsies are positive and 20% of nasal biopsies might show specific GPA findings. In our patient, given the risk of optic nerve compression, treatment was initiated quickly. Nasal biopsy performed few weeks later was negative due certainly to the rapid healing of the lesions.
Cancer incidence was rarely assessed in GPA. Some studies reported an increased incidence of bladder or renal cancers and acute myeloid leukemia assigned to cyclophosphamide treatment [5].
But whether malignancy is a trigger for GPA or not, is not proved yet. Tatsis et al. [6] suggest that malignant cells may participate in the pathogenesis of vasculitis via cytokine production. Faurschou et al. [7] did not find a clear evidence of an increased preceding cancer in a cohort of 293 GPA. In our case we think that such association is no more than fortuitous as prostatic adenocarcinoma is prevalent at that age.
GPA diagnosis can be delayed in case of minor clinical manifestations at the onset of the disease. Clinicians should be aware of such atypical finding as the disease can have a threatening prognostic. The risk of preceding cancer in GPA patients is not proved yet. Systematic screening for malignancy might be indicated in elderly due to its epidemiological prevalence.
The authors declare that they have no potential conflict of interest relevant to this article.
Download Provisional PDF Here
Article Type: CASE REPORT
Citation: Kechida M, Ksiaa I, Rhouma KB, Zaafrane N, Khochtali S, et al. (2018) Bronchiolitis Obliterans Organizing Pneumonia on the Onset of Granulomatosis with Polyangiitis Associated with Orbital Involvement and Prostatic Carcinoma. J Infect Pulm Dis 4(1): dx.doi. org/10.16966/2470-3176.134
Copyright: © 2018 Kechida M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Publication history:
All Sci Forschen Journals are Open Access