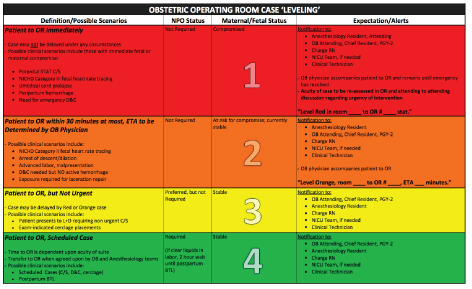
Figure 1: Table demonstrating obstetrical operating room leveling categorization into four levels. Table describes common scenarios, NPO status, maternal/fetal status, and expectations of each team member.

Herng-Yu Sucie Chang1 Nicole Gavin2 Truc-Anh T Nguyen1 Jeanne S Sheffield2 Linda Szymanski2 Jamie Murphy1*
1Department of Anesthesia and Critical Care Medicine, The Johns Hopkins University, Baltimore, Maryland, United States*Corresponding author: Jamie Murphy, Anesthesia and Critical Care Medicine, The Johns Hopkins University, 1800 Orleans Street, Sheikh Zayed Tower 8120, Baltimore, Maryland 21287, USA, E-mail: jmurphy@jhmi.edu
Article Type: RESEARCH ARTICLE
Citation: Chang H-YS, Gavin N, Nguyen T-AT, Sheffield JS, Szymanski L, et al. (2018) A Multidisciplinary Approach to Peripartum Triaging of Patients to the Operating Room. J Clin Anesth Manag 3(1): dx.doi.org/10.16966/2470-9956.137
Copyright: © 2018 Chang H-YS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Publication history:
Objective: At our institution, a triage or leveling system for emergency surgeries in the general operating rooms (OR) exists with the goal of optimizing patient care and reducing morbidity and mortality. In the obstetric field, medical terminology exists for these situations to delineate and convey the urgency of a particular peripartum situation such as “stat, emergent, or urgent”; however, this terminology is not universal and somewhat ambiguous, causing confusion and unnecessary delays in patient care. In this concept paper, we proposed a quality improvement project that delineates terminology for obstetrical triaging to the operating room (OR) and discussed metrics for evaluation of this quality intervention.
Methods: We developed a four-level stratification system to triage patients using clear guidelines for all OR cases. Our system accounted for maternal and fetal stability, indication for surgical intervention, role for obtaining additional studies, nil per os (NPO) status, and surgical and anesthetic concerns. Within each classification, we defined the expectations for each team member’s role, including the obstetrician, anesthesiologist, charge nurse, nursing staff, neonatal intensive care unit (NICU) team, and the surgical and clinical technicians.
Results: Several metrics will be collected to evaluate this multidisciplinary quality improvement initiative, including maternal demographics, labor characteristics, and indication for surgery. Additional data includes level assigned, time to OR, type of surgery performed and anesthetic delivered. We will collect fetal delivery data (Apgar scores and umbilical cord gases), as well as maternal delivery data, including estimated blood loss, time to uterine incision and delivery, and surgical complications.
Conclusions: We propose a multidisciplinary four-category triaging system to delineate the communication and action plan for obstetrical OR cases. We omitted ambiguous terms and developed an algorithm for patients according to acuity and risk. Our quality improvement intervention allows for rapidly changing circumstances and accounts for both obstetric and anesthetic considerations.
The concept of triaging patients originated from the management of military trauma situations where wounded soldiers were systematically evaluated and treated. Triage is the process of prioritizing patient care based on the needs of the patient and the availability of resources. This process has been modified and adopted in hospital systems, most notably in the emergency department and in managing the surgical suite.
At our institution, a triaging (or leveling) system for emergency surgeries in the general operating rooms (OR) exists with the goal of optimizing patient care and reducing morbidity and mortality. Cases are leveled based on surgical acuity with attention to anesthetic concerns, nursing, and resource availability. A level 1 case indicates the need for immediate surgical intervention and the patient is to be in the OR within 60 minutes of the surgical decision.
In obstetrics, triage assessment incorporates both maternal and fetal considerations. Priority is given to situations with obvious threat to life to the mother or to the fetus. While medical terminology exists for these situations to delineate and convey the urgency of a particular peripartum situation, for example “stat, emergent, or urgent,” it is generally acknowledged that this terminology is not universal and is somewhat ambiguous, causing confusion and unnecessary delays in patient care [1]. Furthermore, simply classifying the need for cesarean into a single “emergency” category is insufficient as varying levels of “emergencies” exist. In the modern-day era, the obstetrical decision for surgical intervention prompts the mobilization of a team of providers, including the obstetrician, anesthesiologist, nursing and surgical technicians, and supporting OR staff. Thus, effective communication among team members is essential.
In addition to cesarean deliveries, OR triaging in obstetrics also encompasses surgical or invasive interventions during the postpartum period. Postpartum hemorrhage, vaginal or cervical lacerations, retained products, previously unrecognized placenta accreta, increta, orpercreta, and uterine prolapsed carry varying levels of urgency. There is no current standard of practice for decision to OR intervention for these situations, as is the case for the decision-to-incision for delivery of a neonate.
We propose a quality improvement project which will delineate terminology for obstetrical triaging to the OR via a multidisciplinary approach and discuss metrics for evaluation of this quality improvement intervention.
The most common assessment of the well-being of the fetus is monitoring of the fetal heart rate. Cardiotocography (CTG) couples the electronic monitoring of the fetal heart rate via an ultrasound transducer with the mother’s uterine contractions measured by a pressure transducer placed on the abdomen. This information is generally assessed for a minimum of 20 minutes upon admission of the mother to the obstetrical floor, and the information collected is used to determine the overall well-being of the fetus. A non-reassuring fetal heart tracing, if unable to be corrected with standard obstetric interventions, often triggers the decision for a cesarean delivery, which at times is “emergent”.
Historically, the Fifth Edition of the Standards of Obstetrics and Gynecology published in 1982 stated that “an obstetric service that generally cares for high-risk patients should be staffed and equipped to handle emergencies and to be able to begin cesarean delivery within 15 minutes [2].” Roles were also defined for both the anesthesiologist and obstetrician. After a 1987 study reported that most small community hospitals could perform an emergency cesarean section within 30 minutes [3], the Seventh Edition of the Standards of Obstetrics and Gynecology was revised and extended the 15 minute guideline to a 30 minute decision-to-incision interval [4]. It is important to note that the guidelines indicated that a hospital should be capable of performing an emergency cesarean delivery within 30 minutes; not that 30 minutes should be a standard of care or benchmark for adequate care when cesarean delivery is indicated. In fact, decision-to-incision remains controversial since evidence does not necessarily support improved neonatal outcomes [5]. The Eighth Edition of the Guidelines for Perinatal Care (2017) published by the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics recommends that the “decision to incision interval should be based on the timing that best incorporates maternal and fetal risks and benefits”, requiring communication between obstetrics, anesthesia and pediatric specialties.
To expedite the decision-to-incision process, impactful communication amongst the team is most salient and can be facilitated by agreement of a common vernacular. Lucas, et al (2000) developed a classification to describe the degree of acuity for cesarean delivery: (1) immediate threat to life (maternal or fetal), (2) maternal or fetal compromise that is not immediately life threatening, (3) needing early delivery but no maternal or fetal compromise, and (4) delivery at the convenience of the patient or practice.
The National Institute for Health and Clinical Excellence (NICE) guidelines recommend a dual category classification [6]. Category 1 describes immediate maternal or fetal threat to life with a guideline of 30 minutes to delivery. Category 2 describes maternal or fetal compromise which is not immediately life-threatening with a guideline of 30-75 minutes to delivery. These guidelines are recommended for audit of cases rather than as a standard for clinical care. While these classifications exist, there is no unified language amongst health care providers in practice for conveying vital information regarding the status of the parturient.
The Royal College of Obstetricians and Gynecologists (RCOG) modified the system by Lucas (2000) and proposed a 4-level classification system for cesarean delivery urgency [7]. Recent results evaluating the clinical efficacy of that classification system suggest it was effective at separating clinical situations by risk, ultimately leading to a 30-minute decision to delivery interval in over 90% of true “emergency” cesarean deliveries [1].
As with all decisions that require complex decision-making, communication is critical for a team to function expediently. Though categorizations exist defining the acuity of obstetric situations, clarification regarding definitive time frames for action and specific job descriptions for each team member may improve the quality of care and hopefully maternal and/or neonatal outcomes. On a systems level, these complex decisions and actions are sometimes made within a resource-limited environment. Additional considerations may need to be made depending upon the availability of staff, equipment, facility space, and even the acuity of the unit at the time.
We propose an algorithm for triaging the care of peripartum patients who require surgical intervention. This obstetrical OR leveling system stratifies patients based on the patient’s needs and current resources.
We developed a multidisciplinary stratification system at our institution to triage obstetric patients into a four-level system with clear guidelines for all OR cases. By developing a standardized OR triage system, our goal was to improve communication, remove language ambiguity, and match the needs of the patient with the OR resources and staff availability. Our categorization system accounted for maternal and fetal stability, indication for surgical intervention, role for obtaining additional studies, nil per os (NPO) status, and surgical and anesthetic concerns. We omitted ambiguous terms such as “urgent” and “emergent.” We mandated an alert notifying all pertinent clinical staff that a patient had been identified to go to the OR. Within each of the four classifications, we defined the expectations for each team member’s role, including the obstetrician, anesthesiologist, charge nurse, nursing staff, neonatal intensive care unit (NICU) team, and the surgical and clinical technicians (Figure 1).
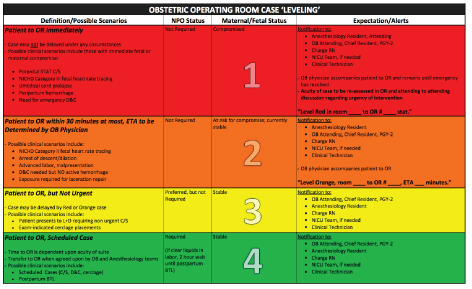
Figure 1: Table demonstrating obstetrical operating room leveling categorization into four levels. Table describes common scenarios, NPO status, maternal/fetal status, and expectations of each team member.
Each level corresponds primarily to threat of maternal or fetal health and is color-based: red, orange, yellow, and green. Once a patient is assigned a category, the triaging continues, unless the category is “red”, and the patient may be reassigned to a different category if necessary after further assessment. For example, if a patient requiring a repeat cesarean delivery presents prior to her scheduled date with premature rupture of membranes but is stable and just ate a full meal, she originally may be triaged as “yellow”; however, if she starts bleeding, she may be changed to either “orange” or “red” depending upon the severity of the bleeding. This leveling system allows for cases of higher priority to supersede cases of lower acuity. This may also lead to better relationships among providers as there will be little ambiguity regarding which case should be done first. Case priority is defined by strict guidelines and the order determined within each level is based on the time of posting.
A level red refers to a case with an immediate threat to the life of the fetus or mother and may not be delayed under any circumstance. Possible clinical scenarios include a National Institute of Child Health and Human Development (NICHD) Category III fetal heart tracing [8,9], umbilical cord prolapsed, peripartum hemorrhage, or emergency dilation and curettage (D&C). The patient should be transported to the OR as soon as possible without delay. Ideally, updated laboratory values, including an active type and screen exist, but the procedure is not delayed if unavailable. These data can be obtained concurrently with ongoing intervention. NPO status is not required since the threat to life of mother and/or fetus outweighs the risk of aspiration. The sequence of events at the time of decision includes direct notification of the obstetrical attending, chief resident and PGY-2, anesthesiology attending and resident who will receive the patient in the OR, charge nurse, NICU team if necessary, and clinical and surgical technicians who will prepare the OR. An obstetrician accompanies the patient to the OR and both obstetrical and anesthesiology teams remain with the patient until the post-operative acute care unit (PACU) phase or the emergency resolves. Once the patient has arrived in the OR, the acuity of the case will be reassessed. A discussion between the obstetrical and anesthesiology attending regarding the surgical and anesthetic approach will occur. The goal of this sequence of events is to expedite patient transport to the OR for immediate intervention with the least amount of delay
A level orange case requires the patient to arrive in the OR within 30 minutes from the time of decision with the approximate estimated time of arrival determined by the obstetrician. In this category, the mother and/or fetus are clinically stable, but the obstetrician identified an elevated risk to the health of the mother and/or fetus without immediate threat to life. Possible scenarios include NICHD Category II fetal heart tracing, arrest of descent or dilation, advanced labor in a patient requiring a cesarean delivery for malpresentation, requirement of D&C with no active hemorrhage, or exposure required for laceration repair. Similar to level red, ideally laboratory studies including an active type and screen are available, but no delay for obtaining these data is recommended as they can be obtained concurrently during the intervention. Appropriate NPO status is not required since risk of compromise to the mother or fetus outweighs the risk of aspiration. Notification requirements include the obstetrical attending, chief resident and PGY-2, the anesthesiology resident, charge nurse, NICU team if needed, and the surgical and clinical technicians. An obstetrician accompanies the patient to the OR, while the anesthesia resident debriefs the anesthesia attending. Once the patient is in the OR, the acuity of the case will be reassessed. The obstetrical and anesthesiology teams accompany the patient to the PACU at the end of the case.
A level yellow case requires operative intervention, but there is no maternal and/or fetal compromise at the time of evaluation. Timing to the OR is agreed upon by both the anesthesiology and obstetrical providers. The case may be delayed if a level red or orange case is identified. Possible scenarios include a patient presenting to labor and delivery who requires a non-urgent cesarean section or examindicated cerclage placement. Ideally, the case is delayed until the patient’s NPO status is appropriate and laboratory studies, including a type and screen, are resulted. The notification process includes the obstetrical attending, chief resident and PGY-2, anesthesiology resident, charge nurse, NICU team if necessary, and the surgical and clinical technicians. The anesthesiology and obstetrical teams remain with the patient from the start of the case until the PACU phase.
A level green case is most dependent on the acuity of the OR suite and unit. The patient and/or fetus are stable with no threat to the health of either. Possible scenarios include a scheduled cesarean delivery, D&C, cerclage, or a postpartum bilateral tubal ligation (BTL). NPO status for these patients is required, as are laboratory studies, including an active type and screen, if indicated. If the patient is in early labor or presents with ruptured membranes and requires a cesarean delivery, she should be NPO for at least 2 hours after clear liquids. Notification includes the obstetrical attending, chief resident and PGY-2, anesthesiology resident, charge nurse, NICU team if needed, and surgical and clinical technician. Patients in this category are at the lowest risk for maternal or fetal compromise; thus, any case with greater acuity may supersede a level green.
Several metrics will be collected to evaluate this multidisciplinary quality improvement project, including maternal demographics, labor characteristics, and indication for surgical intervention. Metrics involving the leveling system will include level assigned, time of patient arrival in OR, and a binary classification of meeting time expectations. Additional data collected include the type of surgery performed and anesthetic delivered. We will also collect fetal delivery data, including Apgar scores and umbilical cord gases, as well as maternal delivery data, including estimated blood loss, time to uterine incision and delivery, and surgical complications. Metrics are assessed biweekly to determine the accuracy of patient classification. An evaluation will ultimately be performed to determine the efficacy of the new system in comparison with the previous system prior to the quality improvement implementation. This foundation can then provide a framework for understanding time to incision intervals and if triaging guidelines can positively affect the health and safety of patients.
We propose a four-category triaging system to delineate and facilitate the communication and action plan for all types of obstetric OR cases. We omitted ambiguous terms and developed an algorithm to categorize patients according to acuity and risk. Our system allows for rapidly changing circumstances and accounts for both obstetric and anesthetic considerations.
Our categorization is based on the previously described 30-minutedecision-to-incision interval, though the literature is controversial regarding the efficacy of this arbitrary interval in improving maternal and/or neonatal outcomes. In a large, multicenter study of women undergoing emergency cesarean delivery, decisionto-incision intervals of less than 30 minutes (versus 30 minutes or more) were associated with higher rates of fetal acidemia and neonatal compromise, confirming the need for expedited delivery [10,11]. Importantly, 95% of the neonates in the 30 minute or more group did not experience adverse outcomes and maternal complication rates were also similar between groups. Similarly, a systematic review and meta-analysis concluded that there was no convincing evidence to suggest that neonatal morbidity was worse when the decisionto-incision interval was more than 30 minutes [5]. The authors also reported that delivery within 30 minutes was not achieved in a substantial proportion of these emergency cases. Regarding maternal outcomes with emergency cesareans, it is important to note that a recent meta-analysis reported significantly increased maternal complications [12]. Importantly, studies do support improved neonatal outcomes with expeditious delivery (even sooner than 30 minutes) in true emergencies or what would be classified as Level Red in our system. Examples include uterine rupture [13] and placental abruption [13,14]. This emphasizes the importance of a leveling system, resulting in immediate transport to the OR with Level Red cases, rather than a 30-minute rule.
Emergency surgeries also involve anesthetic concerns, including choice of neuraxial anesthesia or general anesthesia. The most recent Practice Guidelines for Obstetrical Anesthesia from the ASA Task Force on Obstetrical Anesthesia note that neuraxial techniques (epidural, combined-spinal epidural, and spinal) are associated with improved maternal and fetal outcomes when compared to general anesthesia (GA) [6] though consideration of each individual patient’s medical co morbidities is critical, as well as the need for expedient anesthetic delivery. Neuraxial technique may be contraindicated in cases of patient refusal, coagulopathy, and/or thrombocytopenia. Preexisting neurologic conditions and vascular malformations may alter the decision process in favor of general anesthesia, as well as history of difficult and prolonged neuraxial attempts, patients with prior instrumentation of the back, or presence of high body mass index. The risk of difficult airway and aspiration pneumonia significantly decreases with neuraxial anesthesia and this technique minimizes the exposure of the neonate to anesthesia. In cases where a patient’s NPO status can be optimized, the risk of aspiration significantly decreases and should be taken into account when considering prioritization of the case. For situations where surgical intervention for impending (but not immediate) maternal or fetal compromise is indicated, risks of GA would preferably be avoided.
The mortality of GA compared to neuraxial has significantly decreased over the years, from a risk ratio of 16.7 in 1985-1990 to 1.7 in 1991-2002 [6]. The risks of GA in the obstetrical population are not insignificant with complications from anesthesia being the 6th leading cause of mortality in the US [6]. These risks include inability to ventilate or intubate, difficult intubation potentially worsening fetal hypoxia, maternal aspiration pneumonia, and postoperative respiratory depression. Exposure to volatile agents increases the risk of uterine atony and subsequent bleeding. Fetal exposure to anesthetics via placental transfer increases the risk of fetal respiratory depression and apnea. Although it has been recommended that GA is the preferred anesthetic choice in a “category 1” cesarean section [7], we encourage dialogue between the anesthesiologist and obstetrician to determine the fastest method for appropriate anesthesia. In select patients, this is often administering spinal anesthesia.
In conclusion, we propose a multidisciplinary quality improvement project for effective triaging of patients using a four-category, colorcoded leveling system to the obstetrical ORs. Data from this quality improvement project will facilitate a systems-based approach to streamlining communication and delivery of obstetrical care to patients. A 4-level system may also allow for more appropriate delivery timing compared with an arbitrary 30-minute rule.
None
Download Provisional pdf here
All Sci Forschen Journals are Open Access